COVID-19: What Can PAs Do to Help?

Plus, a COVID-19 CDC resource list at the end of the post!
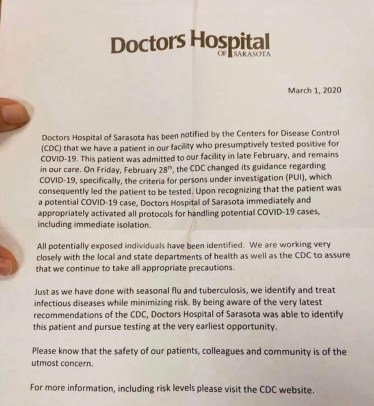
Last night, as our house was winding down, my husband received a text from one of his work colleagues… one of our local hospitals has quarantined a patient from the county I live in, who was presumed positive for “Coronavirus Disease- 2019” also known as COVID-19. Later that evening, I saw that another presumed patient is just an hour north of my home. Our governor has declared a state of emergency because of this, and as we speak my home is literally surrounded by the first known COVID-19 patients in our state.
I’d been pretty casual about COVID-19 up to this point. As a Physician Assistant (PA), I knew that the early data suggested that influenza was more deadly, and after knowing of the local pediatric deaths from Flu, I’d been preaching about the importance of vaccinations and handwashing for quite a while. It wasn’t until I started seeing my social media feeds blow up that I realized, the mass hysteria is about to start. We can’t help but share the news, which I fear only increases the levels of anxiety we all feel. I’m equally guilty of course, sharing and texting to my closest friends and colleagues, but started to realize, a lot of confusion still exists! So, my PA friends, I’ve set out to give you the facts as I understand them!
According to the CDC: “A presumptive positive case has tested positive by a public health laboratory and is pending confirmatory testing at CDC”. This likely means it is only time before an increase in the frequency of testing starts occurring. Since COVID-19 looks like the common cold in the majority of patients, I anticipate it’s going to be a busy few weeks in our local hospitals, clinics, and offices.
Why are people making such a big deal about COVID-19?
My personal opinion is because it’s new, exotic, and people fear the unknown. Experts are trying to compile what data they have to make recommendations, and so the information is ever-changing. Fear-Mongering and social media has made the situation worse, certainly, and the only real way to combat it is by presenting the facts, and pointing people to the CDC and WHO resources (lots of links below).
What Can I Do To Help As A PA?
Be Informed and Only Share the Facts
As a PA, people may look to you for guidance and suggestions. Arm yourself, your family, your friends and your patients with facts. Reassure them of the things they can do to prevent the spread of illness, and remind them that most people with COVID-19 have mild disease and will recover!
Key points about COVID-19:
- Most (80%) of people infected with COVID-19 virus have mild to moderate disease and recover
- The name of the virus is actually ” SARS-CoV-2″ and the disease it causes is “Coronavirus Disease 2019” (abbreviated “COVID-19”)
- There are many types of Coronaviruses, most of which present similarly to the common cold. Reports of fever, cough, shortness of breath, fatigue, malaise have been reported according to this WHO report. The severe and critical cases clinically have what looks like severe pneumonia.
- Those at highest risk are over 60 years and those with underlying conditions such as hypertension, diabetes, cardiovascular disease, chronic respiratory disease and cancer. Disease in children appears to be relatively rare and mild with approximately 2.4% of the total reported cases reported amongst individuals aged under 19 years. A very small proportion of those aged under 19 years have developed severe (2.5%) or critical disease (0.2%)
- It has an incubation average of 5-6 days (also from WHO report) but technically symptoms can present up to 14 days after exposure.
- As of March 2, 2019, the CDC reports that there are 10 states reporting cases in California, Oregon, and Washington. According to some of the media reports, in the past 24 hours, I’ve seen cases reported in Florida and New Hampshire. This number will likely increase over the next few weeks as we increase testing.
Remember what you learned in epidemiology!
- R0
- One of the big concerns is the R0 (pronounced”R naught”) which is what represents the reproduction number, or the ability of a disease to infect others. Measles has an R0 of 12-18, Seasonal Influenza has an R0 around 2-3, 2009H1N1 has an R0 of 1.4 and Ebola 1.5-2.5 (data according to Joseph Eisenberg, Professor and Chair of Epidemiology, University of Michigan).
- The R0 of the Wuhan Coronavirus 2019 ranges from around 1.4 to 4. This number will likely change (and hopefully decrease) as more data comes in, but it’s clear that it might be more contagious than influenza. I’ve read that until the R0 dips below 1.0, then it’s likely the disease will continue to spread.
- Case Fatality Rates (CFR)
- The other concern was the mortality rate or “Case Fatality Rate”. It is often reported as a percentage, so one can infer that a CFR of 1% means that 1 person out of 100 would die from the illness and so on. Severe seasonal influenza has a CFR around 0.1%, and some of the influenza pandemics of 1957 & 1968 had CFRs around 9%. SARS has a CFR of 10% and MERS has a CFR of 39%.
- A New England Journal Article suggests the Case Fatality Rate for COVID-19 is around 1-2%, but that number continues to move as more data comes in.
Review and Know Your Employer’s Plan
Do you know what to do if someone walks through your doors with fever and shortness of breath stating they were exposed to a patient with COVID-19? Now is the time to review your policies, ask questions and know what to do. Use the CDC’s suggestions on steps healthcare facilities can take now to prepare.
- Run through some mock scenarios with your team. Ask questions, point out flaws, and work on a plan. Include a plan for a “surge”, meaning a patient influx that is greater than your team can manage.
- Inventory your equipment. Do you have enough gowns, masks and gloves? Remember you’ll be planning to limit exposure to these patients, but everyone who sees them must wear protective gear. Do you have an isolation room? Where will these patients go when they arrive?
- Make sure your entire team knows about this plan. A simple email to the team with a summary can save a lot of questions later, plus, you want everyone on the same page!
Other Ways PAs Can Help Our Patients
- Encourage the patients you are seeing RIGHT NOW to ask questions about COVID-19, even if that is not the purpose of the visit. This is likely to spread, so the earlier you start the better. Ending a visit by asking the question may trigger their memory, dispute any false information or fear-mongering and help reassure them!
- Use Word or Google Docs to make handouts for patients with simple information to give them facts, answer questions, and tell them what they should do if they develop symptoms. They don’t have to be fancy, or lengthy!
- Send the document out as emails, snail-mail, and give to each patient you see
- Make sure there is plenty of signage in your department or office, notifying patients to put on a mask when appropriate, and that they should notify someone if they are concerned they have COVID-19. Assure that there is plenty of waiting room supplies such as hand sanitizer, tissues, and masks as needed.
- And then there are the obvious things. Don’t go to work sick. Wash your hands, and wear the appropriate protective gear (see below!)

What type of Personal Protective Equipment (PPE) do I need?
Last October I took a Hospital Emergency Response Team (HERT) course where we learned some of the basics of how to manage mass casualty events, which doesn’t exactly apply here but the principles of sudden onset of increased patient load, the importance of keeping patients in isolation, “donning” and “doffing” personal protective gear are similar. Just to be clear, so far we do not require the pictured level C gear for gross decontamination for COVID-19! CDC recommends standard, contact and airborne precautions which includes:
- N95 respirators- make sure they fit well!
- gowns- don’t forget to tie in the back
- gloves- consider double gloves
- face shield/eye protection or goggles. Glasses do not count!


Encourage Patients to Use Telehealth & Virtual Medicine Services When Appropriate
The CDC suggests that patients who are mildly ill with COVID-19 are able to isolate at home during their illness. Obviously, those who are short of breath, or concerned should seek medical care (and start by calling and giving the facility a warning they are coming with concern for COVID-19) but for those who think they can stay home but want to speak to a medical provider, I am a huge fan of the concept of Telehealth/Virtual Medicine in these circumstances! You may recall an interview with Desmond Watt, who is a strong advocate for PAs in Virtual Medicine and Telehealth. If a patient’s provider offers these services, then I’d encourage patients to use them!
- KinderDoc is a trusted telehealth resource and is owned by an awesome Pediatrician whom I worked with in our busy Pediatric ER (and he gets bonus points, as his wife is a PA!). It started as a pediatric telehealth resource but now, his team will see patients of all ages! The first visit is $30.. that’s a no brainer in my book.
A COVID-19 CDC Resource List:
I went through the site and pulled out what I think are the most helpful links from the CDC! I encourage you to spend some time looking up these things… if you work clinically, this will definitely impact you!
- Situation Summary– talks about the current state of COVID-19
- Information for Healthcare Professionals– a good place to start for PAs
- Evaluating and Reporting Persons Under Investigation– How and when to test for COVID (this link should continue to remain updated)
- Clinical Care – how to care for COVID-19 Patients (hint, it’s mostly supportive)
- Resources for Healthcare Facilities– is your hospital or office following these recommendations? Be proactive by reviewing the recommendations and seeing how you can help.
- Travel Recommendations– you may have your own travel concerns, or your patients might. This link provides a map, and the most up to date travel restrictions related to COVID-19
CDC Printouts:


I hope that this post becomes completely obsolete and that COVID-19 turns into a Y2k scenario, but if not, I hope it was helpful! If there’s some other great resource or infographic you’d like to share, please reach out and we’ll add it! Until then, stay safe my friends!
Courtney
All statements are my personal opinion and do not represent medical advice! Please follow the recommendations of your employer, state, or national guidelines for COVID-19.



